As tuberculosis cases rise in the US and worldwide, health officials puzzle over the resurgence of a disease once in decline
An outbreak of tuberculosis, or TB – a lung disease that is often accompanied by a hacking cough – began in January 2024 in Kansas City, Kansas, and two nearby counties and continues as of early March 2025. To date, 147 people have been reportedly diagnosed with TB in the outbreak, with 67 becoming ill. The remaining 80 people diagnosed with TB in Kansas contracted the illness but showed no symptoms, which is called a latent infection.
TB is the leading infectious cause of death around the world, outpaced only by COVID-19 during the first three years of the pandemic.
The Conversation asked microbiologists Karen Dobos and Marcela Henao-Tamayo, both from Colorado State University, to explain why this ancient disease seems to be making a comeback.
What’s the history of TB?
Mycobacterium tuberculosis is the organism that causes the disease tuberculosis in humans. The disease has been infecting humans for thousands of years. Researchers found evidence of the disease 9,000 years ago in the excavated remains of people who lived in the Eastern Mediterranean region during that time.
Reports of TB date back to around 410-400 B.C.E., when the physician Hippocrates termed the disease phthisis, an archaic word that means a progressive “wasting away,” due to the way people with the disease become emaciated.
TB was also known as consumption for the same reason. Similarly, it was called the white plague or white death – due to anemia from the disease, with people appearing pallid or chalky – leading to near-certain death. Untreated active TB, meaning cases that are symptomatic, is highly lethal.
About half of all people with untreated active TB die from the disease, whereas treatment reduces the death rate to 12%.
One of the more colorful phrases describing TB is “the king’s evil.” This is a form of TB that also causes neck swelling and lesions, a condition called scrofula. During the Middle Ages, people believed that the touch of a king could cure a person from this form of TB through miraculous intervention.
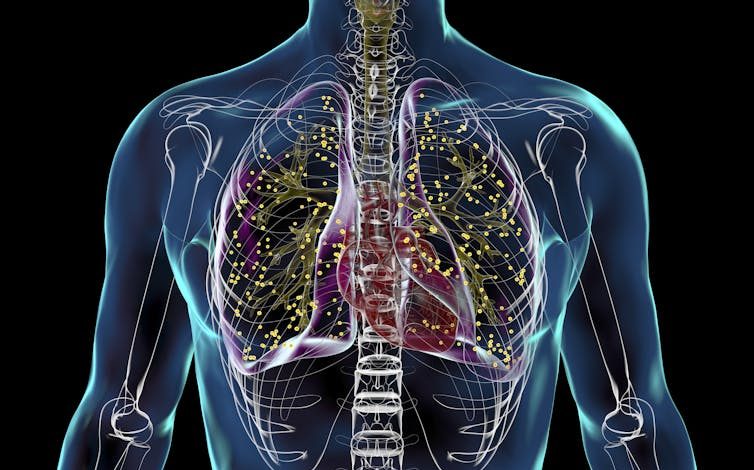
Kateryna Kon/Science Photo Library via Getty Images
Finally, TB was most ominously called the “robber of youth” due to its historical propensity to afflict people 15 to 30 years old.
In 1865, Jean Antoine Villemin, an army physician in Paris, demonstrated that TB could be transmitted from infected animals to healthy ones through inoculation. Before these studies, the cause of TB was presumed to be primarily constitutional, by either an inherent predisposition or from unhealthy or immoral lifestyles.
The microorganism causing TB was ultimately discovered in 1882 by the German physician Robert Koch. Koch announced his findings on March 24, 1882, a day globally recognized as World TB Day.
How does TB spread?
Tuberculosis is spread by small infectious droplets in the air. A TB patient may emit these droplets by coughing, singing and potentially from regular breathing that occurs during sleep or resting.
One form of TB can be spread through unpasteurized dairy products. While rare, there have been reports of TB transmission through bone graphs, in which healthy, donated bone material is used to replace damaged bones.

Kateryna Kon/Science Photo Library via Getty Images
The origin of the TB outbreak in Kansas remains unknown as of early March 2025. The outbreak has disproportionately affected those in low-income communities, and two people have died from it.
Importantly, a patient with untreated TB can infect 10 to 15 others.
Could the COVID-19 pandemic be a factor?
The COVID-19 pandemic has played a pivotal role in the resurgence of TB. Cases increased globally by 4.6% from 2020 to 2023, reversing decades of steady declines in the disease. In the U.S. alone, TB cases rose by more than 15% from 2022 to 2023.
During mandatory shutdowns, people were less able to access health care centers for early diagnosis of TB or to fill prescriptions for treatment, perhaps due to the fear of contracting COVID-19 while visiting a medical care facility. COVID-19-related disruptions in care resulted in nearly 700,000 excess deaths from TB.
Access to health care may not be the only factor behind this uptick. Medical supply shortages and delays in shipment may have also played a role. For example, the U.S. experienced shortages of one of the primary TB drugs between 2021 and 2023.

Smith Collection/Gado/Archive Photos via Getty Images
What are the main treatments?
Multidrug treatment is currently the only way to cure TB and stop its spread.
Prior to the late 1930s, when the first antibiotic for TB treatment was developed, TB treatments included bloodletting and consumption of cod liver oil. The most popular treatment involved isolated sanatoriums in high-altitude areas such as the Adirondacks and the Rocky Mountains, where the cold, dry air was believed to be a cure. Scholars at the time suggested that the potential for cure was due to these environments being more invigorating for the body and providing more restful sleep. There is no evidence to support these beliefs.
Streptomycin was the first antibiotic treatment to become available for TB, in the 1940s. However, the microorganism quickly became drug resistant. A second antibiotic, called isoniazid, was developed as a first-line treatment against TB in the 1950s. Again, the microorganism became drug resistant.
Two- and four-drug combinations are now used to treat both latent infections and active disease. Treatment of active TB requires at least six months of uninterrupted therapy. Disruptions in treatment result in further spread of TB and the emergence of multidrug resistant TB, which requires additional drugs and more than nine months of treatment.
All TB drugs are toxic; the quality of life for TB patients deteriorates during treatment and remains so throughout their lives. Finding cases and treating TB illness early, before symptoms begin, is important because it not only reduces the spread of disease but also greatly reduces drug toxicity.
What should people be aware of?
People should be aware that TB is still a public health problem across the globe. Education on the transmission, treatment and need for active work to eradicate TB is the best defense.
One of the reasons why education and awareness about TB are so important is that a person with latent TB may be unknowingly harboring the microorganism for years. In the absence of symptoms, these people are unlikely to seek care and will not be diagnosed and treated unless identified as part of an outbreak, as was the case for more than half of the patients in Kansas.



